Dying from Dysphagia
Written on November 12th, 2017 by Napassorn
Ever had trouble swallowing? Probably not. This conditions only affects 1 out of 17 people. But as you get older, the chances become higher.
What is Dysphagia?
Dysphagia or trouble swallowing might seem as a trivial medical issue. But despite procedural diagnosis and consistent monitoring using a flexible endoscope, more than 60,000 adults in the US die per year. Any one of us can die from this. It can be me; it can be you.
Any condition that causes weakness or damage to the muscles and nerves used for swallowing may lead to dysphagia. This includes diseases such as Parkinson’s, throat, head and neck cancer, side effects from head injuries or stroke, or even just getting old. These conditions inhibit proper neuro-muscular movement and/or control during the swallowing process. As a result, in these patients, food and liquid residue is left over in the throat after swallowing. Such residue can cause a reduction in quality of life, a need to change what and how people eat (in turn causing weight loss, dehydration), and even pneumonia if the residue falls into the airways into the lungs.
Current Diagnosis Approach and its Flaw
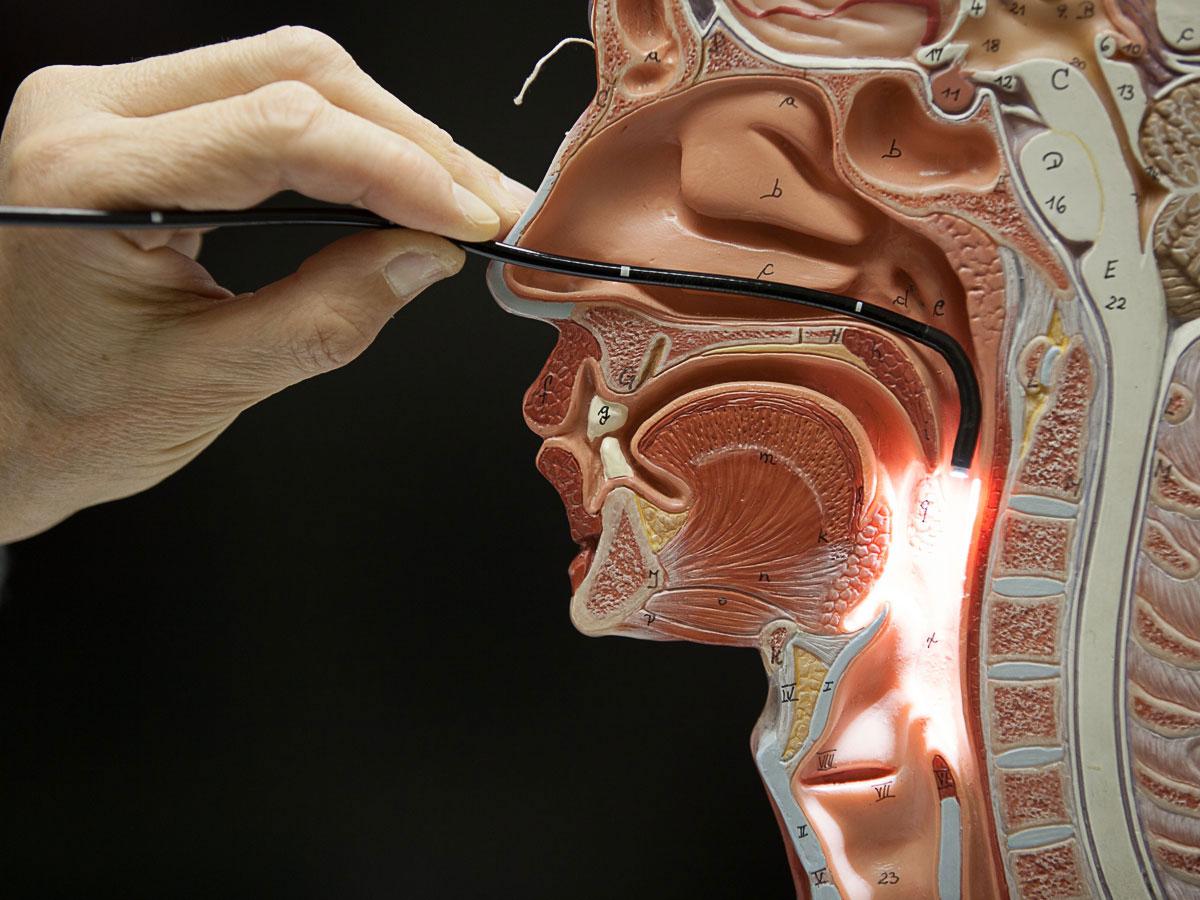
Currently, the severity of dysphagia can be assessed visually via a 2D flexible endoscope that is inserted into a patient’s nose and then advanced into their pharynx. However, there is no objective or quantifiable way to measure how much residue is left in a patient’s throat. Clinicians must simply “guess” how much residue is in the throat using their best intuition and experience. This ultimately leads to inconsistent and subjective severity assessments of dysphagia among clinicians, which in turn prevents the meaningful measurement of a patient condition.
It’s like having Doctor A tell the patient that he/she has “somewhat severe” condition of dysphagia and Doctor B telling the same patient that he/she has a “very severe” condition. What does that even mean to the patient? How do doctors treat him/her then if each has their own opinion on the level of severity? How would doctors discuss this patient’s condition with others when there is no standard criteria?
Ultimately, such a subjective analysis is an enormous issue for clinical evaluation, documentation, and communication. If only we had someway of quantifying this condition. Imagine Doctor A and B both read from the computer that the patient has 70% severe dysphagia. They are no longer “guessing” because a program is actually calculating severity for them. But with the 2D nature of a standard endoscopic image, such quantification of the 3D anatomy of the hypopharynx is difficult. If only there is a 3D flexible endoscope out there.
Luckily, my senior project team is teaming up with a research assistant professor at Boston University School of Medicine (our client) to do exactly that and ultimately, help change the way doctors diagnose and treat dysphagia!
See how our client is manufacturing the world’s first 3D flexible endoscope here. (Insert link)
See how my senior project team are creating the software application the works with the 3D endoscope to compute quantifiable results like described above here.